|
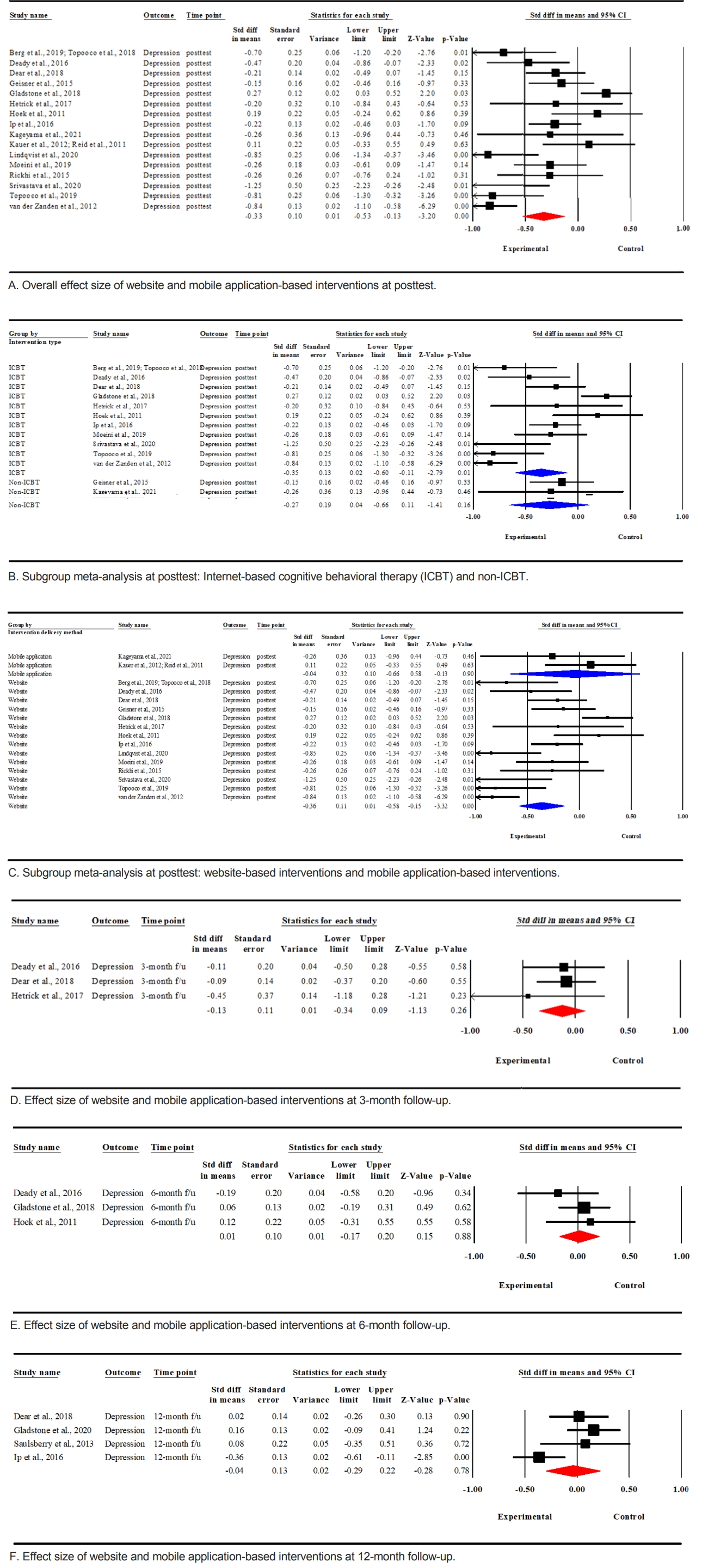
Berg et al. (2019); Topooco et al. (2018) |
Sweden |
Adolescents scoring 14 or more on the BDI-II and exhibiting at least five symptoms or fulfilling the MDD diagnosis according to the MINI 6.0 |
N=70; 94.0% female; adolescents: 15 to 19 years |
ICBT and chat-based psychological support to treat adolescent depression; chat and web-based; eight skill-based modules and chat sessions for eight weeks |
Attention control (monitoring and non-specific counselling) receiv- ing treatment after the post-treatment assessment |
BDI-II, PHQ-9 |
Baseline, posttest |
|
Deady et al. (2016) |
Australia |
Young people with current moderate depression symptomology, with a score of seven or more on the DASS-21 |
N=104; 59.6% female; adolescents: 18 to 25 years |
The self-help intervention named DEAL (DEpression-ALcohol) project based on the SHADE (Self-Help for alcohol/other drug use and Depression) program (consisting of evidence-based CBT and motivational interviewing) to treat depressive symptoms and problematic alcohol use; web- based; four sessions for four weeks |
Attention control (health watch) |
PHQ-9 |
Baseline, posttest, three and 6-month follow-up |
|
Dear et al. (2018) |
Australia |
Young adults with a self-reported, principal complaint of depression or anxiety symptoms |
N=192; 81.8% female; adolescents: 18 to 24 years |
The Mood Mechanic Course (ICBT) using online lessons to treat anxiety and depression symptoms in addition to a weekly contact from a clinician; web-based; four lessons for five weeks |
The Mood Mechanic Course and a self-guided treatment (no clinical contact) |
PHQ-9 |
Baseline, posttest, three and 12-month follow-up |
|
Geisner et al. (2015) |
United States |
College students with a depressed mood (a score of 14 or higher as measured by the BDI-II) |
N=311; 62.4% female; undergraduates: 18 to 24 years |
Intervention 1: alcohol intervention consisting of personalized feedback and brief psychoeducation for the potential relationship between alcohol and depressive symptoms |
Assessment-only control (view information for depression and substance use without any personalized feedback or intervention materials) |
BDI-II |
Baseline, posttest |
|
Intervention 2: mood intervention consisting of personalized feedback and strategies for coping to treat depressive symptoms |
|
Intervention 3: integrated inter- vention consisting of a combination of both the alcohol intervention and depressive symptoms inter- ventions; web-based; five weeks |
|
Gladstone et al. (2020); Gladstone et al. (2018); Van Voorhees et al. (2020) |
United States |
Adolescents with elevated symptoms of depression and/or a history of a major depressive episode or dysthymia |
N=369; 68.0% female; adolescents: 13 to 18 years |
The CATCH-IT program to prevent or reduce depressive symptoms; web-based; 15 and five adolescent and parent modules, respectively |
Attention control (the Health Education intervention that provides general health information) |
CES-D-10, DSR |
12, 18, and 24 months |
|
Hetrick et al. (2017) |
Australia |
Young people who experienced suicidal thoughts in the past four weeks |
N=50; 82.0% female; adolescents: 13 to 19 years |
The TAUand Reframe-IT based on the Internet-delivered standard CBT approach focusing on suicidal thinking and behaviors; web-based; eight modules for 10 weeks |
TAU |
RADS-2, CDRS-R |
Baseline, posttest, 3-month follow-up |
|
Hoek et al. (2011); Richards et al. (2016); Saulsberry et al. (2013) |
United States |
Adolescents experiencing persistent subthreshold depression (having one core depression symptom for at least a few days in the last two weeks at both the initial screening and one to two weeks later at the eligibility assessment) |
N=84; 56.6% female; adolescents: 14 to 21 years |
Motivational interview and CATCH-IT program via internet for preventing depression; web-based; 14 modules |
Primary care physician brief advice and CATCH-IT program via internet |
CES-D-10, PHQ-A, clinically significant depressive episodes |
Baseline, 6-week, 6-month, 12-month, and 2.5-year follow-up |
|
Ip et al. (2016) |
Hong Kong |
Adolescents at risk of depression with scores of 12~40 on the CES-D |
N=257; 68.1% female; adolescents: 13 to 17 years |
Grasp the Opportunity (modified CATCH-IT) to reduce negative cognition and behaviors, improve resiliency, and strengthen positive behaviors; web-based; 10 modules for eight months |
Attention control (access to an anti-smoking website without depression intervention) |
CES-D, DASS-21 depression subscale |
Baseline, 4- (interim), 8- (posttest), and 12-month follow-ups |
|
Kageyama et al. (2021) |
Japan |
People scoring 16 or more on the CES-D |
N=32; 34.4% female; adolescents: 18 to 24 years |
Intervention using video viewing smartphone including positive word stimulation; smartphone application; 10 minutes of daily video viewing (at least 70 min weekly) for five weeks |
Wait-list control receiving the intervention after the five-week outcome measurement |
CES-D |
Baseline, posttest |
|
Kauer et al. (2012); Reid et al. (2011) |
Australia |
Adolescents in the early stages of depression with mild or more severe emotional or mental health issues assessed by a general practitioner or by scoring more than 16 on the K10 |
N=118; 72.8% female; adolescents: 14 to 24 years |
Mobile phone self-monitoring program to assess and manage mental health problems; mobile phone application; eight modules for two to four weeks |
Attention control (receiving an abbreviated version of the mobile-type program without ESA and mental health modules) |
DASS-21 depression subscale |
Baseline, posttest, 6-week follow up |
|
Lindqvist et al. (2020) |
Sweden |
Adolescents diagnosed with unipolar major depressive disorder in accordance with the DSM-5 criteria (a score of 10 or higher as measured by QIDS-A17-SR) and the MINI 7.0 |
N=76; 80.0% female; adolescents: 15 to 18 years, |
Affect-focused internet-based psychodynamic therapy to improve emotional avoidance, awareness, experience, and expression of emotions with therapist support; web-based; eight modules for eight weeks |
Supportive control (weekly contact via Internet with the symptoms and well-being monitoring) |
QIDS-A17-SR, MADRS-S |
Baseline, posttest, 6-month follow-up assessed only by the intervention group, and not the control |
|
Moeini et al. (2019) |
Iran |
Adolescents with mild to moderate depressive symptoms, with scores of 10 to 45 on the CES-D |
N=243; All female; adolescents: 15 to 18 years |
Web-based depression improvement program based on social cognitive theory to manage mild and moderate depression; web-based; seven modules for six months |
Usual curriculum |
CES-D |
Baseline, mid-treatment (3 months), posttest (6 months) |
|
Rickhi et al. (2015) |
Canada |
Adolescents and young adults with a mild to moderate severity according to the DSM-IV-TR criteria for MDD, with a raw baseline score 40~70 in CDRS-R (adolescents) and 12~24 on the HAM-D (young adults) |
N=31; 83.8% female; adolescents: 13-18 years |
Spirituality-informed intervention for mental health based on principles including forgiveness, gratitude, and compassion; web-based; eight modules for eight weeks |
Waiting-list control receiving the intervention initiated after an eight-week waiting period |
CDRS-R (adolescents), HAM-D (young adults) |
Baseline, posttest (8 weeks), 16 and, 24 weeks |
|
N=31; 58.0% female; young adults: 19 to 24 years |
|
Srivastava et al. (2020) |
India |
Adolescents with an ICD-10 diagnosis of mild or moderate unipolar depression |
N=21; 23.8% female; adolescents: 13 to 19 years |
Smartteen—a computer-assisted CBT program to treat adolescent depression; web-based; 12 sessions for 12 weeks |
TAU receiving the intervention after the post-treatment assessment |
BDI-II, CDRS-R |
Baseline, mid-treatment (6 weeks) posttest (12 weeks) |
|
Topooco et al. (2019) |
Sweden |
Adolescents with depressive symptoms (14 or more points on the BDI-II), and presenting at least four symptoms including one core symptom, or fulfilling the criteria for a major depressive episode according to the MINI |
N=70; 96.0% female; adolescents: 15 to 19 years |
ICBT and chat-based psychological support to treat adolescent depression, including major depressive episodes; text- and web-based; eight ICBT modules and eight individual therapist sessions delivered through chat for eight weeks |
Minimal attention control receiving treatment after a posttreatment assessment |
BDI-II |
Baseline, posttest, 12-month follow-up assessed only by the intervention group, not the control |
|
Van der Zanden et al. (2012) |
United States |
Adolescents and young adults with a score between 10 to 45 on the CES-D |
N=244; 84.4% female; adolescents: 16 to 25 years |
Grip op Je Dip (Master Your Mood) based on the CBT group course for young people with symptoms of depression; web-based; six weekly sessions |
Waiting-list control receiving the intervention after a 14-week waiting period |
CES-D |
Baseline, posttest (3-month), 6-month assessed only by the intervention group, not the control |