Development of a Self-Reported Communication Competence Questionnaire for Patients with Schizophrenia
Article information
Abstract
Purpose
To develop a self-reported communication competency scale for patients with schizophrenia.
Methods
Twenty-nine preliminary items were selected from 42 candidate items derived from literature review and qualitative interviews using content validity analysis of expert opinions to evaluate 637 patients’ schizophrenia communication competence. Data from 383 individuals were analyzed. Confirmatory factor analysis was conducted using data of 280 individuals. The final dataset included data from 254 participants. Data were subjected to exploratory and confirmatory factor analyses using SPSS and AMOS 24.0.
Results
After evaluating the model fit index for the last 24 items, the following results were obtained: x2=633.95 (p<.001), x2/df (degree of freedom)=2.26, SRMR=0.04, RMSEA=0.06, TLI=0.93, CFI=0.94, NFI=0.96. Therefore, this tool’s suitability was evaluated as acceptable. The final scale comprised 24 items and 3 subscales that could measure basic, interpersonal, and communicative expression of patients with schizophrenia.
Conclusion
A self-reported communication competency scale was developed for patients with schizophrenia. It is expected to help measure the effectiveness of intervention programs to improve communication among patients with schizophrenia.
INTRODUCTION
We communicate with many people daily. It is challenging if we do not communicate with people in our lives. Communication can help us know when, where, and how to speak. It helps us exchange information with others, give value to others, and react internally and externally [1]. In other words, it is the ability to effectively express thoughts and feelings using language, symbols, texts, and media suitable for various situations. It refers to the ability to correctly understand the thoughts and feelings expressed in words and writings of others, listen to and respect opinions of others, and mediate conflicts effectively [2].
However, patients with schizophrenia show cognitive deficits in various areas due to the disease, significantly affecting their communication [3,4]. Schizophrenia is a typical mental illness that occurs mainly in people in their 20s and 30s. It is rarely cured within a short period . About 70% of diagnosed patients become chronic through continuous symptom onset and repeated recurrence [5]. As the disease becomes chronic, negative symptoms such as poor or inconsistent verbal expression, decreased emotional expression, lack of spontaneous conversation, loss of interest in social interaction, inappropriate response to situation, regression, and withdrawal appear [6,7]. For them, inappropriate communication decreases emotional expression. Inappropriate responses that do not fit a situation can cause communication problems [8]. This communication disorder is most commonly experienced by patients with schizophrenia, among other mentally ill patients, leading to social isolation due to chronic difficulties in social interaction and problems in interpersonal relationships [8]. Communication disorders in patients with schizophrenia can directly lead to their difficulties in interpersonal relationships and social adjustment, even if symptoms improve. Communication disorders in patients with schizophrenia is a significant cause of repeated hospitalization [9,10]. Since patients with schizophrenia experience difficulties and conflicts in interpersonal relationships due to communication problems, communication training programs are being implemented to solve these problems.
Tools such as “Marital Communication Measurement,” “Adolescent Empathy Tool,” and “Interpersonal Relations Measuring Tool” can be used to evaluate the effectiveness of a communication training program after simple vocabulary correction and supplementation work [11,12]. However, as communication characteristics between patients with schizophrenia and the general public are very different, it is difficult to use communication measurement tools for ordinary people with only simple vocabulary correction and supplementation. In addition, as it is difficult to measure characteristic deficits in communication of patients with schizophrenia, a communication competency measurement tool for patients with schizophrenia is needed.
Most tools developed to measure communication in patients with schizophrenia have been designed to identify communication problems. In addition, Communication Disturbance Index, a tool that could measure a concept similar to communication, has been developed [13]. However, the tool has low reliability [14] as subjective analysis is possible. In addition, among tools frequently used in clinical practice, it is a general purpose for measuring communication in patients with schizophrenia when the Diagnostic and Statistical Manual of Mental Disorders (DSM -4) is applied using Global Assessment of Functioning (GAF) measures [15]. However, the GAF score is limited in measuring communication because it evaluates various factors such as apathy, communication difficulties, and lack of self-management, which are overall indicators of vocal symptoms with a single score. Thus, it is not being used frequently [16].
One instrument has been developed in Japan to measure communication in patients with schizophrenia [17]. However, its use is challenging as it does not fit the domestic psychiatric environment. In addition, it is not a self-report questionnaire [18]. Furthermore, it is challenging to use tools developed abroad directly in Korea because understanding of items may change due to cultural differences in vocabulary expression when using tools developed abroad. Therefore, it is necessary to objectively evaluate a program’s effectiveness in reducing recurrence of patients with schizophrenia becoming pendent in daily life and develop a systematic tool to understand the communication ability level of patients with schizophrenia. Thus, the objective of this study was to develop a self-reported communication competency scale for patients with schizophrenia to understand the communication ability level of patients with schizophrenia and to assess the effectiveness of an intervention program. Its reliability and validity were then evaluated.
METHODS
1. Research Objective
This methodological study aimed to develop a tool for measuring communication competency of patients with schizophrenia and to verify its reliability and validity.
2. Research Process
1) Tool development process
(1) Components and initial question compositions
① Literature review
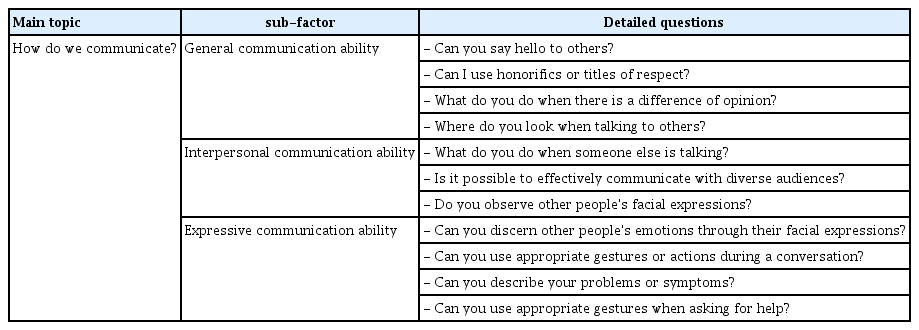
This study reviewed domestic and foreign literature to examine the concept of communication and its sub-components. This study focused on interpersonal and nonverbal communication. Based on sub-factors of communication ability derived from literature review and communication characteristics of patients with schizophrenia, this study will develop a tool with three sub-concepts: "general communication ability," "interpersonal communication ability," and "expressive communication ability."
A review of relevant domestic and international literature was conducted to identify communication issues faced by patients with schizophrenia. PubMed, MEDLINE, and CINAHL were searched. Domestic literature was searched at RISS4U, KISS, and the Library of Congress. Keywords were searched by combining different words such as 'schizophrenia and/or communication', 'schizophrenia empathy', 'schizophrenia interpersonal relationship' and 'psychosis communication'. In addition, by studying books on schizophrenia, we were able to identify anatomical and physiological issues associated with the condition as well as communication characteristics of patients with schizophrenia. We also learned about effective approaches for communicating with these patients. Based on this, we constructed semi-structured interview questions that could reflect communication characteristics of patients with schizophrenia (Appendix 1).
② Focus group interview
A focus group interview was conducted to confirm conversation patterns of patients with schizophrenia. Selection criteria for interview participants were the same as those for the preliminary focus group interview participants. There were seven interview participants. For focus group interviews, all contents were used until no new data were obtained. The average age of participants was 52.8 years and the average length of hospitalization was 10.3 years. Focus group interviews were conducted directly by a researcher with ten years of experience as a psychiatric ward chief nurse and 12 years of experience as a professor in charge of psychiatric nursing. The interview was conducted one-on-one after the content of discussion was thoroughly explained and consent was obtained. At the beginning of interviews, two or more individual interviews were conducted to form a rapport with the patient after a specific time. The first interview took approximately 40~70 minutes. Data were transcribed and analyzed immediately after the interview. Missing information was added during the second interview while checking the report.
③ Preliminary tool development
Preliminary questions were completed based on constituent factors derived in the first step. In this study, essential tool items were prepared from 42 meaningful data points from a literature review and focus group interviews with schizophrenia patients. Preliminary questions consisted of three sub-areas: 15 questions on “daily communication ability,” 15 questions on “interpersonal communication ability,” and 12 questions on emotional communication ability. Tool items were evaluated with a 5-point Likert scale. Preliminary questions were completed based on constituent factors derived in the first step. In this study, essential tool items were prepared from 42 meaningful data points from a literature review and focus group interviews with schizophrenia patients. Preliminary questions covered three sub-areas: 15 questions on "daily communication ability," 15 questions on "interpersonal communication ability," and 12 questions on emotional communication ability. These questions were evaluated with a 5-point Likert scale.
(2) Content validity
Content validity of the first set (42 preliminary items) was tested by a panel of three psychiatrists, five professors of nursing, and three mental health nurses with extensive experience in tool development. Opinions were collected regarding any incomprehensible sentences, ambiguous expressions, words that were difficult to interpret, and further questions that needed to be added. Agreement of panel members was estimated using a item-level content validity index (I-CVI) and a scale-level content validity index (S-CVI/Ave). The content validity of an item was determined as suitable for selection if the I-CVI score was ≥0.78 and the S-CVI/Ave score was ≥90 [19]. Eight items were removed, including the following items with I-CVI < 0.80: "When talking to other people, you can start the conversation first"; "I hear a deadpan voice when talking to others"; "I can describe my family's symptoms related to my illness." In addition, a total of 13 items, including 2 items for conversation with family, 2 items for disease management, and 1 item for polite expressions, were deleted based on expert opinion that they were redundant or unsuitable for schizophrenia patients.
2) Tool validation process
(1) Participants
Selection criteria for study participants were as follows: 19 years of age or older, diagnosed with schizophrenia by a mental health professional according to the DSM-5 diagnostic criteria, did not receive a dual diagnosis such as drug or alcohol addiction other than schizophrenia, and had symptoms at the time of data collection. Participants who were judged by their attending physician to be cooperative and capable of answering the survey, as well as those who understood the purpose of this study and agreed to participate, were included. Under the assumption that the number of participants in the tool development study should be at least 100 and 7 to 10 times the number of items required for exploratory factor analysis [20], the total number of participants was determined to be 390, which was 8 times the initial 42 questions, considering a dropout rate of 15%. Data from 383 (98.2%) participants were analyzed, excluding 7 participants who answered survey questions insincerely or left many questions unanswered.
For secondary data collection, the sample size was determined to be 240 participants based on the recommendation that a minimum of 200 participants would be required for confirmatory factor analysis (CFA) [21]. Considering a dropout rate of 15%, a total of 280 people were recruited. Among these, data from 254 (90.7%) people were used in the study, excluding data from 26 individuals who answered survey questions insincerely or had a high number of unanswered questions.
(2) Data collection
Preliminary tools developed in this study were verified by a psychiatric ward, a psychiatric hospital, a psychiatric rehabilitation facility, and day hospital systems of university hospitals located in two provinces that researchers and research assistants could easily access. Data were collected from patients with schizophrenia at 11 locations. Data collection for this study was conducted twice. The first period was from December 1, 2020 to February 28, 2021. The second period was from March 14, 2021 to June 1, 2021.
(3) Ethics statement
For ethical consideration of patients, contents and methods of this study were approved by the institutional research ethics review committee of the researcher's affiliated university hospital and each institution for data collection (IRB NO: **UH 2019-11-006-00). The purpose of this study was explained to the director and permission was obtained from all participants. Patients who used a ward, center, or facility with data collection approved by the attending physician were recruited. Patients who expressed their intention to participate in this study were informed the purpose of this study and that: 1) contents of this research and collected data would be used only for research purposes; and 2) they could withdraw from this study at any time.
(4) Statistical analysis
Data analysis of this study was performed using SPSS/WIN 25.0 and AMOS 26.0 (IBM Corp., Armonk, NY, USA) statistical programs. Participants’ general characteristics were calculated as frequency, percentage, mean, and standard deviation. Content validity of the tool was evaluated using a 4-point Likert scale from the expert group and calculated using the I-CVI. To verify construct validity, EFA was performed first. After confirming whether the collected data was suitable for factor analysis by performing Kaiser-Mayer-Olkin (KMO) and Bartlett sphericity tests, items with an eigenvalue of 1 as the standard were evaluated for items with communalities of 0.40 or more and factor loadings of 0.50 or more. Factors were extracted for (Peters et al. 2019) Confirmative factor analysis was performed to investigate the structure of the sub-region. In the confirmatory factor analysis, validation of model fit was performed using the x2 statistic (p-value), x2, the absolute fitness index for evaluating overall fit/df, Standardized Root Mean Residual [SRMR], and root mean square error of approximation (RMSEA), taking into account simplicity of the model, the primary Tucker-Lewis Index (TLI), Comparative Fit Index (CFI), and Normal Fit Index (NFI), which are relative fit indices to evaluate the fit of a proposed model. Next, a multi-trait/multi-item matrix analysis was conducted to investigate convergent and discriminant validity of questions. To assess reliability, internal consistency reliability was measured using Cronbach’s ⍺ value, the most commonly used method.
RESULTS
1. Participant Characteristics
Regarding general characteristics of participants in this study, primary data collection subjects for exploratory factor analysis had 224 (58.5%) men and 159 (41.5%) women. The most common age was 50~59 years, accounting for 35.2% (n=135). Regarding marital status, 83.8% (n=321) were single (including separated, widowed, and single) and 16.2% (n=62) were married. Regarding educational background, 53.0% (n=203) had graduated from high school. The onset period was 21 years or longer for 49.8% (n=190) subjects. Regarding current residence, inpatients accounted for the most at 52.7% (n=202), followed by rehabilitation centers at 29.8% (n=114) and day hospitals at 17.5% (n=67). Subjects of secondary data collection for confirmatory factor analysis had 173 (68.2 %) men and 81 (31.8%) women. The most common age was 50~59 years, accounting for 37.0% (n=94). Regarding marital status, 69.3% (n=176) were single (including separated, widowed, and single) and 30.7% (n=78) were married. Regarding educational background, 53.9% (n=137) had graduated from high school. The onset period was 21 years or longer for 59.2% (n=145) subjects. Regarding current residence, inpatients accounted for the most at 51.0% (n=125), followed by rehabilitation centers at 32.7% (n=80) and day hospitals at 16.3% (n=40) (Table 1).
2. Construct Validity
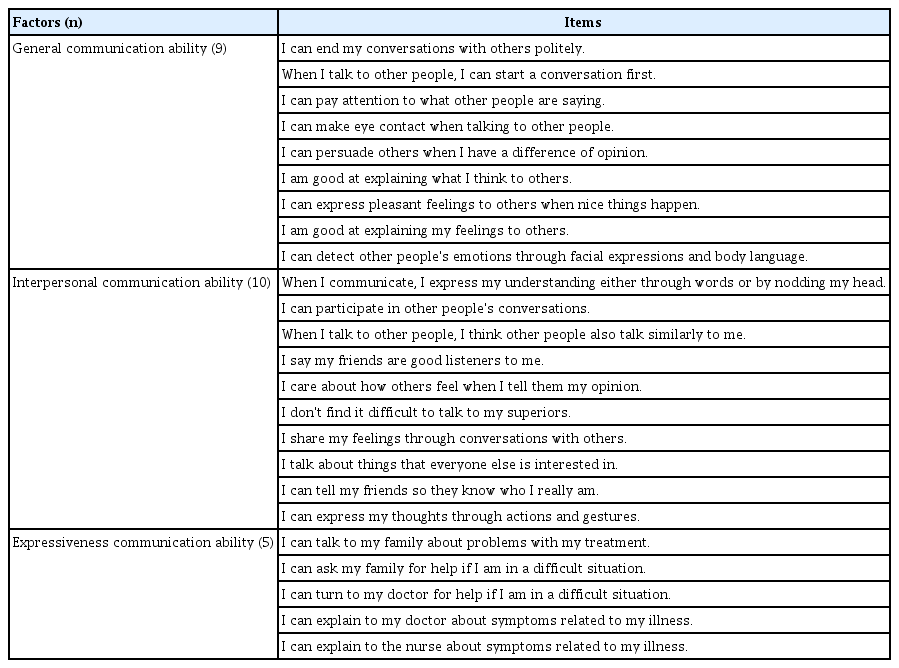
1) Item analysis
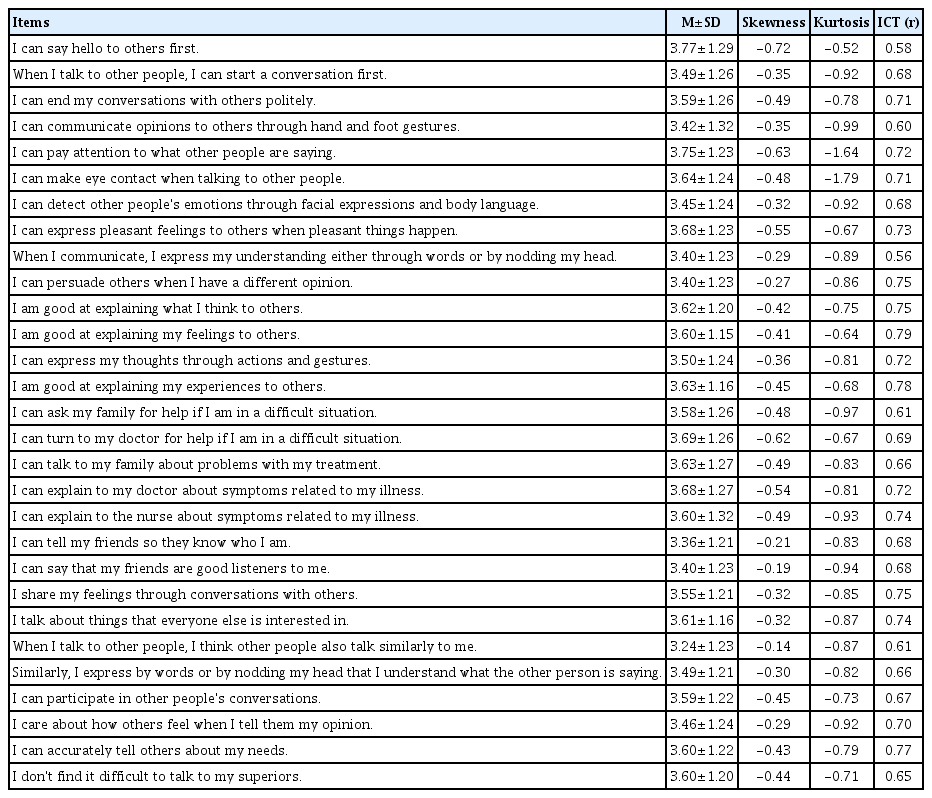
Item analysis was first performed to evaluate items in the tool. As a result of analyzing items, the average score of items was 3.24~3.77. The skewness was -0.72~-0.14 and kurtosis was -1.79~-0.52, showing a normal distribution in all items. No items needed to be deleted. As a result of analyzing corrected item-total correlation coefficient between individual items and all items, the correlation coefficient was 0.50 or higher, confirming the internal consistency of items. Therefore, all 29 items were selected and used for a Communication Competency Questionnaire for patients with Schizophrenia (CCQS) (Table 2).
2) Exploratory factor analysis
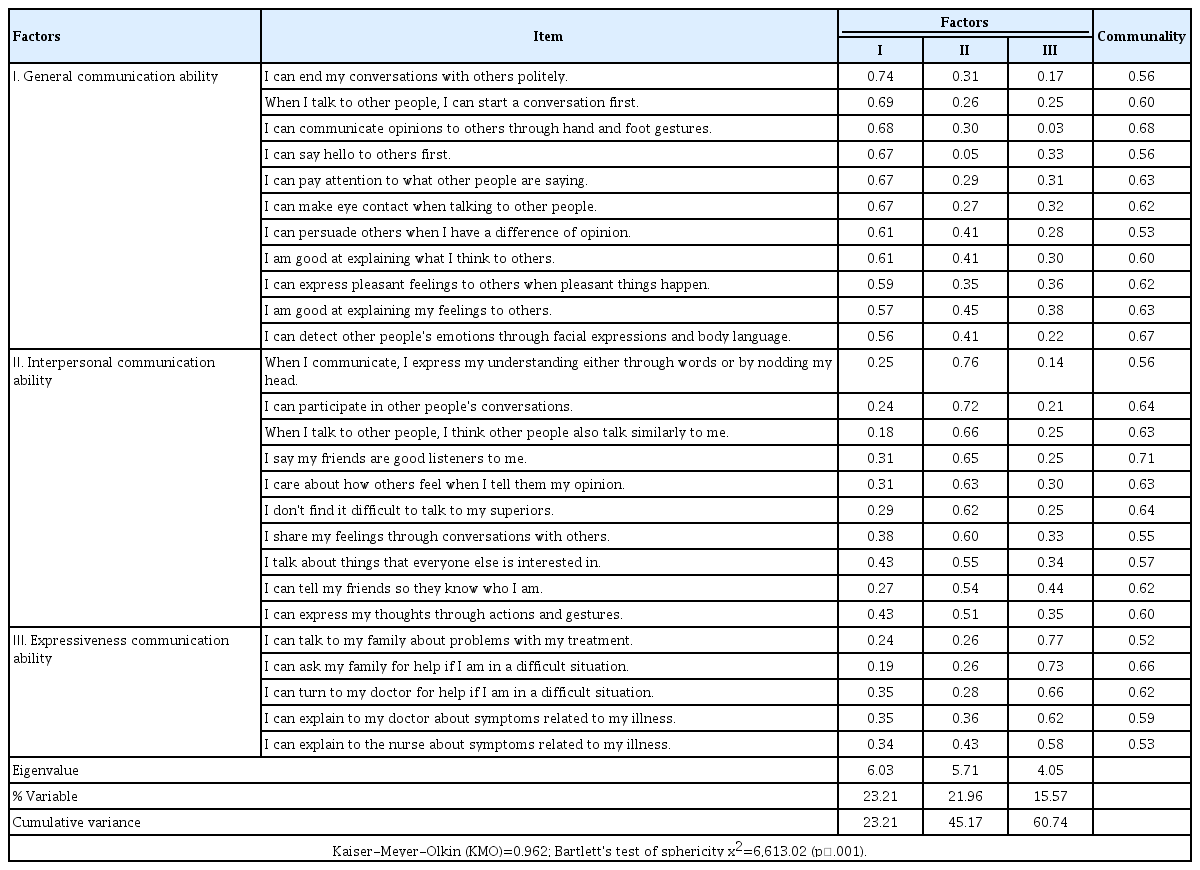
After checking items' internal consistency and content validity, EFA was calculated to verify construct validity (Table 3). As a result of performing the Kaiser-Meyer-Olkin (KMO) test to determine whether the sample was appropriate for factor analysis, KMO value was 0.962 (reference value 0.50), close to 1. Bartlett’s sphericity test was performed to determine whether the correlation coefficient matrix was suitable for factor analysis. Results showed x2=6,613.02 and p<.001, confirming that the correlation coefficient matrix was ideal for factor analysis. Principal component analysis (PCA) is an effective method for identifying construct validity. Thus, PCA was performed for factor analysis. PCA is a suitable approach for this purpose because it is focused on factor clustering. Varimax orthogonal rotation was used to ensure independence between factors and make the developed tool practical and user-friendly.
As criteria for determining the number of factors, three factors were extracted by referring to an eigenvalue of 1 or more and the slope of a scree plot. Questions with a commonality of more than 0.30 and an absolute value of the maximum factor loading of more than 0.50 were selected [2]. Items that were repeatedly found to be appropriate for the above conditions by checking commonalities and factor loadings were deleted. Items 10, 16, and 40, which showed a total commonality of .30 or less. Therefore, it was deleted. As a result of re-checking the commonality and factor loading of the 26 items across the 3 sub-factors, no additional items were found to be included.
The cumulative explained variance was 60.74%. Factor loadings ranged from a minimum of 0.52 to a maximum of 0.81, with the 1st factor explaining 23.21% of the variance, the 2nd factor explaining 21.96% of the variance, and the 3rd factor explaining 15.57% of the variance (Table 3).
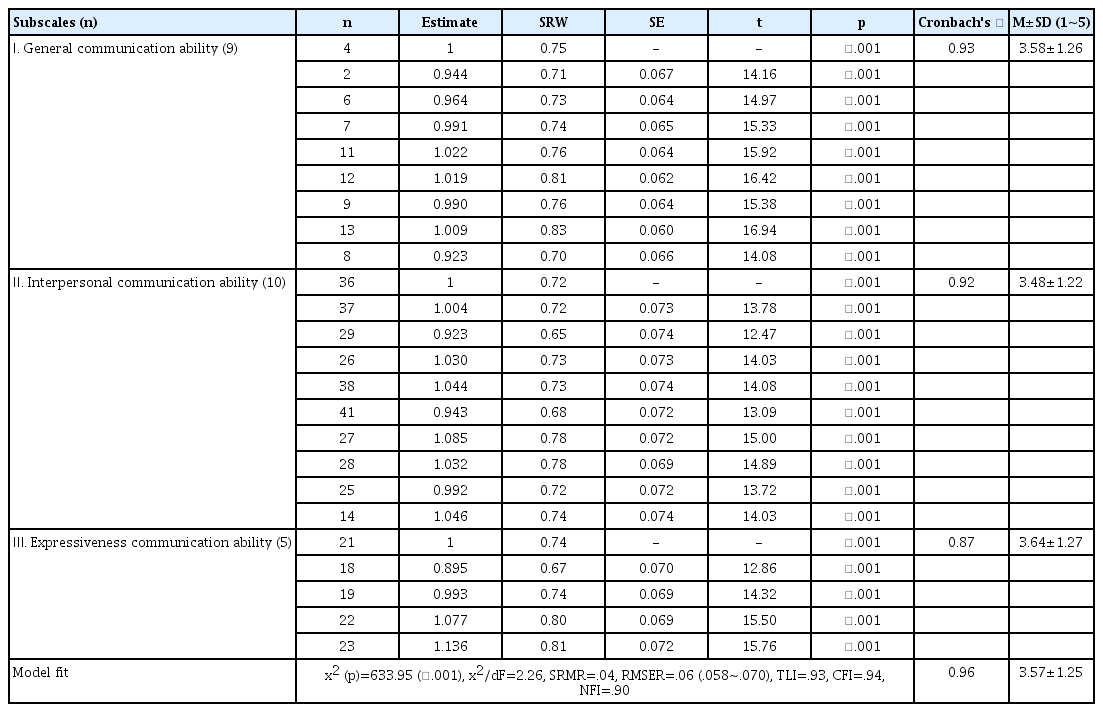
3) Confirmatory factor analysis
Confirmatory factor analysis was conducted on the three sub-factors identified in the exploratory factor analysis using additional data collected from a sample of 378 participants (Table 4). Standardized regression weight (SRW) was analyzed to test the validity of sub-measurement variables for each factor. For confirmatory factor analysis, SRW was first analyzed to test the validity of sub-measurement variables for each factor. As a result, two questions were deleted as they were found to have SRWs less than 0.5. After deleting the two questions and examining the SRW in detail, the SRW ranged from 0.70 to 0.83 for factor 1, 0.65 to 0.78 for factor 2, and 0.67 to 0.81 for factor 3. In conclusion, the tool developed in this study demonstrated a high level of reliability.
CFA model verification was performed based on Goodness-of-Fit Index (GFI), Standard Root Mean square Residual (SRMR), Root Mean Square Error of Approximation (RMSEA), Tucker-Lewis Index (TLI), and Normed Fit Index (NFI). The model fit could be judged to be good if GFI, AGFI, NFI, and TLI are 0.90 or greater and SRMR and RMSEA are 0.05 or less [10]. After evaluating the model fit index for the last 24 items, the following results were obtained: x2=633.95 (p<.001), x2/df (degrees of freedom)=2.26, SRMR=0.04, RMSEA=0.06, TLI=0.93, CFI=0.94, and NFI=0.96 (Table 4).
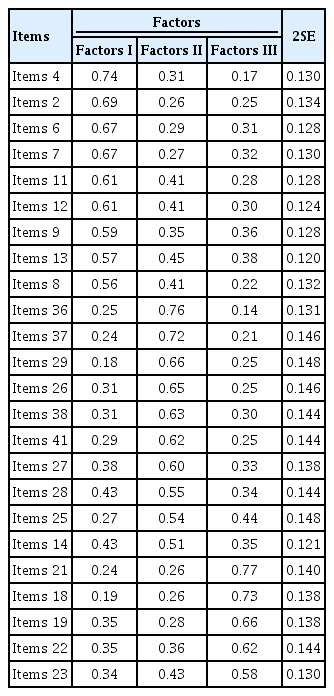
4) Convergent and discriminant validity of CCQS-24 items
The convergent and discriminant validity of CCQS-24 items were tested using a multi-trait multi-item matrix analysis. Results showed that the correlation coefficient between the 24 items and subscales to which each item belongs spanned from 0.50 to 0.77, with all of them being 0.40 or above, indicating that the item's convergent validity was 100% successful (Table 5). In the item's discriminant validity, the correlation coefficient with other subscales to which each item did not belong ranged from 0.14 to 0.45. No item had a value greater than the correlation coefficient compared to the factor to which each item belonged. At the same time, the discriminant validity of the items was established if there was a difference in the correlation coefficient between each item and its corresponding subscale, as well as the correlation coefficient with other subscales. Furthermore, each subscale's Cronbach’s ⍺ coefficient was higher than correlation coefficients among other subscales. Thus, features of each subscale were distinct. Therefore, the item-discriminant validity success rate was 100% (Table 5).
3. Reliability Verification
To evaluate the reliability of the tool, we calculated internal consistency reliability using Cronbach’s ⍺. As a result, Cronbach’s ⍺ value for all 24 questions was 0.96. The change in Cronbach’s ⍺ value when items were removed was 0.93~0.94. Thus, the range of variation was not large. This indicated that the scale had a high level of internal consistency. There were no questions that significantly affected the internal consistency. Cronbach’s ⍺ values of subdomains were 0.93, 0.92, and 0.87 (Table 4).
DISCUSSION
This study aimed to develop a Communication Competency Questionnaire for patients with Schizophrenia (CCQS-24). Finally, an instrument with 3 factors and 24 items was developed. Many intervention programs have been applied to improve communication of patients with schizophrenia in Korea. However, a tool to measure this effect has not been established yet. Therefore, this study is expected to help measure the effectiveness of intervention programs to improve communication of patients with schizophrenia. This study used exploratory and confirmatory factors to verify construct validity. Initially, 42 items were derived. They were first verified for content validity by a group of experts. After excluding duplicate and difficult-to-understand items, 24 items were finally derived through a confirmatory factor analysis and several confirmations. The number of items in the tool for patients with schizophrenia should not be too large considering their short concentration [22]. Therefore, if the current 24 questions could be improved and shortened to 10 to 12 questions in a short version through future studies, its clinical utility will be higher.
After conducting the KMO test before factor analysis, it was determined that the KMO value was appropriate. This indicates that the correlation between variables was well explained by other factors. The contribution of a single factor to the overall variation with practical significance is called cumulative explanatory variance. The cumulative explanatory variance in this study was 60.74%, which was satisfactory. Looking at each factor of this tool, the first factor was named "General Communication Ability." This corresponded with the essential role of communication. It can be seen as the most fundamental communication skill, which is the ability to effectively convey one's message to others and establish connections through conversation. However, schizophrenia patients have problems with this essential communication competency. Thus, their interpersonal relationships are gradually lost [10]. An interpersonal relationship means a person-to-person relationship that gives and receives mutual help. Improving interpersonal relationships is very important for patients with schizophrenia who have a therapeutic goal of interacting with society and living an independent life [10]. Therefore, it is important to have basic communication skills so that measurable interpersonal relationships could be formed. This factor included items of "I can end my conversations with others politely."’ and "When I talk to other people, I can start a conversation first."’
Ten items were selected for the second factor of "Interpersonal Communication Ability." Looking at characteristics of these items, they consisted of inquiries that could assess listening and conversational abilities across different topics. Patients with schizophrenia lack empathy when communicating with others. They do not understand other people's emotions. They cannot adequately express their own emotions, which further reduces their social functioning [12]. Therefore, it is essential to understand other people's emotions and express their own emotions as they aim to maintain stable interpersonal relationships while maintaining an independent life and returning to society [18]. Additionally, negative symptoms can further regress the expression of emotions. Thus, interventions to improve them should be applied. Since items of this sub-factor consisted of contents that could enhance empathy while concentrating on the conversation, it could help evaluate patients’ intervention programs. This factor included items of "When I communicate, I express what I understand verbally by speaking or nodding my head" and "I can actively participate in conversations with other people.”
For the third factor, five items were selected for "Expressive Communication Ability." These items could evaluate listening and communication skills of various subjects. They consisted of inquiries about whether patients could articulate their symptoms and categorize medical personnel (such as nurses and doctors) and family members. This is similar to a study conducted by Takahashi et al. (2006). They found that the communication ability of schizophrenia patients varied depending on the subject. They identified 'interpersonal communication ability' as a sub-factor when developing a tool for patients. In this study, a subfactor was also constructed within the same context.
In other words, schizophrenia is a chronic disease. It is beneficial to have a clear understanding of its symptoms and side effects of drugs in order to determine the appropriate treatment approach and communicate with them effectively. Although side effects of antipsychotic medications manifest in various ways, patients tend not to disclose them. Therefore, it is necessary to educate them on how to communicate their experiences. In addition, intervention programs such as drug education, social skills training, and cognitive behavioral therapy should be implemented in clinical practice to address positive or negative symptoms, such as hallucinations and delusions that might manifest openly [5]. Therefore, it is believed that this tool can be effectively used to evaluate the effectiveness of these intervention programs. In addition, it is believed that this tool can be used for schizophrenia patients. It is distinguished from communication tools used for the general public.
Factor loading in EFA represents the level of correlation between each factor and variable. As all questions in this study had factor loadings ≥0.5, the significance was substantial. Furthermore, for the reliability of the tool developed in this study, Cronbach’s ⍺ values ranged between 0.86 and 0.92 for each factor. The reliability of the tool for the last 24 items of this tool had a Cronbach’s ⍺ of 0.96, indicating very high reliability. Generally, the smaller the number of items, the lower the reliability [2]. However, when this tool was reduced from the initial 42 items to the final 24 items, it showed a high Cronbach’s ⍺. Cronbach’s ⍺ for each of the three factors also showed a value of .80 or more, indicating sufficient reliability. Thus, it was considered as a stable tool. Considering that an ⍺ ≥.60 adequately confirms the reliability of an exploratory study [23], the CCQS-24, which measures the communication skills of patients with schizophrenia, is judged to be appropriate in terms of reliability. Additionally, the CCQS-24 does not contain heterogeneous items. Thus, participants can obtain consistent responses. Questions can also be considered as comprehensive measures. In particular, among sub-factors, interpersonal communication ability is thought to differ between a measured value reported by the patient and a value measured by medical personnel. Therefore, a further study is needed to increase the reliability of the tool by confirming the correlation between the two measures.
The fit of this tool was confirmed through confirmatory factor analysis. Errors for items 1 and 5 exceeded one. Thus, these items were deleted. As a result of evaluating the model fit index for the last 24 items, CFI free from sample characteristics is recommended rather than GFI for model fit [2]. This study showed a CFI of 0.94, which was higher than the CFI standard of 0.90. It satisfied all other conditions. Therefore, the suitability of this tool was evaluated as an acceptable level [20]. Concept reliability for convergent validity is a criterion for assessing concentrated validity. It evaluates whether the indicator properly measures the intended concept [2,20]. Analysis of the convergent and discriminant validity of the CCQS-24 items using multi-trait multi-item matrix analysis revealed 100% convergent and discriminant validity, indicating that items consistently measured construct concepts and that factor independence was preserved. The scale has 24 items evaluated with a 5-point Likert scale ranging from 1 (Strongly disagree) to 5 (Strongly agree).
CONCLUSION
In this study, a communication ability measurement tool was developed for patients with schizophrenia. The reliability and validity of the developed tool were confirmed. Therefore, the tool developed in this study can measure communication abilities of patients with schizophrenia. However, it has the following two limitations. First, due to its self-report nature, there might be discrepancies between results reported by the patient and those assessed by the medical staff. Second, criterion validity was not assessed during the evaluation process for validity. This needs to be confirmed through further research.
Notes
The authors declared no conflicts of interest.
AUTHOR CONTRIBUTIONS
Conceptualization or/and Methodology: Song, EJ & Park, SK
Data curation or/and Analysis: Kwak, YB & Park, SK
Funding acquisition: Song, EJ
Investigation: Kwak, YB & Park, SK
Project administration or/and Supervision: Song, EJ
Resources or/and Software: Park, SK
Validation: Song, EJ & Park, SK
Visualization: Kwak, YB & Park, SK
Writing: original draft or/and review & editing: Song, EJ & Park, SK