The Effects of Patient Safety Culture Perception and Safety Control on the Patient Safety Management Activities of Psychiatric Ward Nurses
Article information
Abstract
Purpose
To provide basic data to find ways to increase the patient safety management activities of psychiatric ward nurses and establish measures for patient safety.
Methods
The research was conducted with psychiatric nurses who had worked for > 6 months in 9 psychiatric hospitals across 3 regions. Data collection spanned June 16 to July 7, 2022, the research tools being patient safety culture perception, safety control, and patient safety nursing activities.
Results
A hierarchical regression analysis showed the factors influencing patient safety management activities. In Model 1, factors of the position of the subject and number of accident reports in the past year appeared significant (F=6.63, p<.001); the explanatory power was 9.8 %. In Model 2, patient safety culture perception appeared significant (F=15.26, p<.001); explanatory power increased to 45.1 %. In Model 3, safety control appeared significant (F=14.63, p<.001); explanatory power increased to 46.6 %. Among the perceptions of patient safety culture, communication, and procedures, incident-reporting frequency and hospital environment were identified as significant.
Conclusion
The factors for psychiatric nurses' patient safety management activities are patient safety culture perception and safety control. Patient safety culture perception is a particularly important factor, and a strategy is needed to increase it.
INTRODUCTION
In today's hospital environment, due to the development of science and the specialization and division of labor in medical services, communication between medical personnel has become complicated, and patient safety accidents occur frequently [1]. The occurrence of patient safety accidents has a negative impact on the health and life of patients, while also extending hospital stay and financial loss, lowering the quality of medical services, and lowering trust in medical staff and hospitals [2]. Therefore, it is vital to prevent accidents that occur in medical institutions.
Psychiatric wards are vulnerable to accidents related to patient safety. Suicide, self-harm, and violence frequently occur in patients admitted to psychiatric wards due to long-term hospitalization and the impairment of thinking, perception, and cognitive functions, and accidents due to suffocation, falls, and the use of restraint devices occur frequently [3,4]. As psychiatric wards are generally closed environments, in the event of a fire or an infectious disease, large-scale casualties and group infections could occur [5]. Psychiatric wards are prone to unexpected accidents, and large-scale damage is likely to occur. Nurses in psychiatric wards should pay more attention to patient safety and accident prevention.
To prevent accidents in psychiatric wards, staff members must be aware of patient safety. Patient safety culture refers to the beliefs, values, and behavioral patterns shared by organizations, departments, and individuals to mini-mize harm to patients [6]. When a patient safety culture is established, not only do patient safety accidents decrease, learning and education about patient safety also take place, and owing to the reduction in patient safety accidents, emotional losses, such as stress and guilt, among medical staff decrease [7]. In the absence of specific guidelines or grounds for nursing, conflicts of opinion in psychiatric wards are likely to occur during the process of nursing, based on experience [8]. However, when a patient safety culture is established, patient accidents can be prevented through active communication and feedback on accidents among ward staff [3].
Safety control is the individual cognitive dimension of safety [9]. It refers to effectively following patient safety management activity (PSMA) guidelines, and making clear judgments about actions against patient safety when placed in a conflict situation [10]. High safety control in nurses has a positive effect on personal and PSMA, both physically and mentally [11]. Psychiatric ward nurses require safety controls to create a safe ward environment by maintaining a balance between protection and control through flexible responses to patients, thereby reducing conflict and tension with patients [12]. However, no studies targeting nurses in psychiatric wards have addressed safety controls.
Psychiatric ward nurses require systematic preventive activities to actively cope with the characteristics of psychiatric patients and their closed environments. PSMA are activities for medical institutions and workers to prevent disasters or accidents that could occur, and refer to systematic activities that can reduce or eliminate risks [13]. The evaluation of mental health institutions includes accurate communication among medical staff regarding patient safety, treatment environment management, emergency management, fall prevention, dining out and accommodation management [14], and systematic and continuous management. Previous studies on PSMA targeting nurses in psychiatric wards are related to the recognition of the medical institution accreditation system [15] and studies on its relationship with patient safety culture perception (PSCP)[3], which can be seen as quite limited. It is necessary to examine both the organizational aspects of PSCP [1-3,7,11] and individual aspects of safety control [9-11] that affect nurses’ PSMA. However, no study has integrated these two variables among psychiatric nurses.
Therefore, in this study, PSCP in the organizational aspect and safety control in the individual aspect were examined to identify the effects of nurses’ safety activities. Further, this study intended to prevent patient accidents by promoting psychiatric ward nurses, and using the results as basic data for developing programs and policies for patient safety.
METHODS
1. Study Design
This descriptive research study investigated PSCP, safety control, and the degree of safe nursing activities in psychiatric ward nurses, and identified factors influencing safe nursing activities.
2. Research Materials and Participants
Participants were randomly selected from nurses who had worked for more than six months in nine psychiatric hospitals located in J province, and K and D metropolitan cities. The sample size was referenced from Cho and Gang [1], the variables used here were similar to those of that study, and the same statistical method was used. The number of participants was calculated using the G*Power 3.1.9 program, and when an appropriate sample size was calculated by setting the number of influencing factors to 5, effect size to .15, significance level to .05, and power to .95 for analysis, 138 participants were required. Considering the high dropout rate of the online survey, the questionnaire was distributed to 200 people. Of these, 157 responded.
3. Instruments
1) PSCP
We used the Patient Safety Culture Hospital Survey Questionnaire [16] developed by the U.S. Department of Health and Welfare, adapted by Je [17] for general nurses, and modified by Kim and Lee [3] to suit psychiatric nurses. This tool has six sub-domains, where each item is rated on a Likert scale ranging from strongly disagree (1 point) to strongly agree (5 points), with higher scores indicating higher PSCP. All the reverse questions were reverse coded (nos. 5, 7, 8, 10, 13, 15, 16, 20, 21, 27, 32, 33, 35~37, 39, and 41). In Kim and Lee [3], Cronbach’s ⍺=.79; in this study, Cronbach’s ⍺=.88, indicating acceptable to good internal consistency.
2) Safety control
This tool was developed by Anderson et al.[9] for office workers, and adapted by Jeong [18] for nurses. It uses a Likert scale with seven questions ranging from strongly disagree (1 point) to strongly agree (5 points), where the higher the score, the higher the sense of safety control. In Jeong [18], Cronbach’s ⍺=.84; in this study, Cronbach’s ⍺ =.87, indicating good internal consistency.
3) PSMA
This tool was developed by Lee [19], and modified and supplemented by Kim and Lee [3] to suit the needs of psychiatric institutions. This tool has six sub-domains, and each question is measured on a Likert scale ranging from strongly disagree (1 point) to strongly agree (5 points), where the higher the score, the higher the level of PSMA. In Kim and Lee [3], Cronbach’s ⍺=.95; in this study, Cronbach’s ⍺=.95, indicating excellent internal consistency.
4. Data collection and ethical considerations
This study was conducted with the approval (no. 1040708-202204-SB-011) of the Institutional Review Board of D University. Data were collected from June 16 to July 7, 2022, after obtaining permission from the head of the nursing department of the psychiatric ward. The questionnaire was self-administered, using a structured Google questionnaire. The questionnaire stated that the collected data did not have personally identifiable information and would not be used for any purpose other than research, and that it could be discontinued at any time. Only those who agreed to the Google survey participated, and after the survey was completed, a small reward was given.
5. Data Analysis
The collected data were analyzed using IBM SPSS 23.0. The general characteristics of the participants were analyzed using frequency and percentage, while PSCP, safety control, and PSMA were analyzed using the means and standard deviations. According to the general characteristics of the participants, PSMA was analyzed using t-tests and analyses of variance, and post hoc analyses were performed using Scheffé test. Pearson’s correlation coefficient was used to determine the correlation between variables, and a hierarchical multiple regression analysis was performed for factors affecting safety nursing activities.
RESULTS
1. PSMA according to General Characteristics
Regarding the general characteristics of the participants, 75.8% were female, 38.2% were aged (41 to 50) years, and 83.4% held a bachelor’s degree or less. For both total work experience and current department experience, 10 years or more was the most common. Professional nursing qualifications accounted for 52.2 % of the participants. In the past year, the percentages of safety training and accident reports were (40.1 and 28.1) %, respectively.
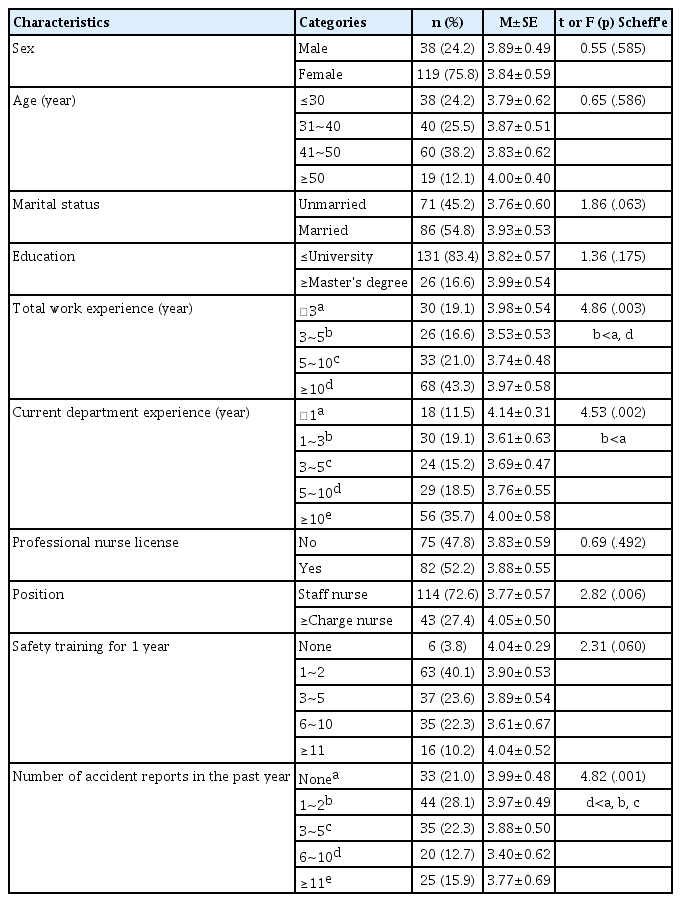
The significant differences in PSMA according to general characteristics were as follows: total experience was higher in those with <3 and ≥10 years than in those with 3~5 years (F=4.86, p=.003). Current experience was higher in those with <1 year than in those with 1~3 years (F=4.53, p=.002). Regarding position, nurses in charge and higher were higher in PMSA than general nurses (t=2.82, p=.006), and the number of accident reports in the past year was higher in 5 cases or fewer than 6 to 10 cases (F=4.82, p=.001) (Table 1).
2. Degree of each variable and its sub-variables
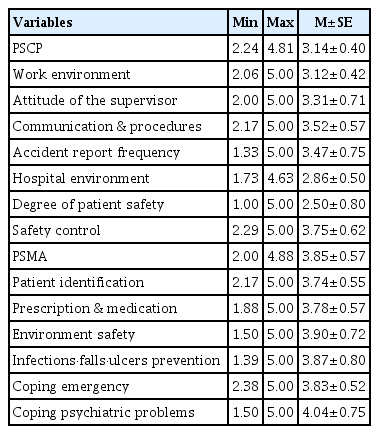
The average PSCP score was (3.14±0.40) points, communication and procedures were the highest in the subdomain, while degree of patient safety was the lowest. The average safety control score was (3.75±0.62), and the average PSMA score was (3.85±0.57) points. In the subdomain, coping with psychiatric problems scored the highest, while patient identification scored the lowest (Table 2).
3. Correlation between Variables
For PSCP and safety control (r=.38, p<.001), PSCP and PSMA (r=.58, p<.001), and safety control and PSMA (r=.36, p<.001), all variables and their sub-domains showed positive correlations (Table 3).
4. Factors affecting PSMA
To determine the factors influencing PSMA activities, a hierarchical multiple regression analysis was conducted by inputting the participants’ work experience in the current department, position, number of accident reports in the past year, PSCP, and safety control. The total work experience of the participants was excluded, because it was similar to the work experience in the current department, and the position was converted into a dummy variable for use.
First, testing the assumptions of the regression analysis found that all the assumptions were satisfied. The tolerance limit was over 0.1, and the variance inflation factor did not exceed 10 for all variables, indicating a multicollinearity problem. Next, as a result of the residual analysis, the linearity of the model, the normality of the error term, and the equal variance were confirmed. In Model 1, participants’ work experience in the current department, position, and number of accident reports in the past year were inputted, and PSMA was explained by 9.8%(F=6.63, p<.001). In Model 2, PSCP was added to Model 1, and PSMA was explained by 45.1%(F=15.26, p<.001). In Model 3, safety control was added to Model 2, and PSMA was explained by 46.6%(F=14.63, p<.001). The factors influencing PSMA were the number of accident reports in the past year, communication and procedures, position, hospital environment, safety controls, and incident reporting frequency (Table 4).
DISCUSSION
This study conducted a hierarchical regression analysis to identify the factors affecting PSMA to prevent accidents and promote safe nursing care in psychiatric wards. Factors affecting the PSMA scores of psychiatric ward nurses are discussed based on the results of the regression analysis.
The general characteristics affecting PSMA were the position and number of accident reports in the past year. The PSMA score was higher for charge nurses than for general nurses, which was consistent with previous studies [11,15,20]. The case where the number of accident reports was less than 5 times in the past year was significantly higher than the number of (6~10) times, and the PSMA score was the highest in “no case”. In previous studies [3,15], when the number of accident reports in the past year was high, PSMA score was also high, which differed from the current results. Notably, the lower the number of accident reports, the higher the PSMA score, as the PSMA helps prevent patient safety accidents. Among the PSMAs for psychiatric nurses, “coping with psychiatric problems” had the highest score, followed by “prescription and medication” and “patient identification”. “Environmental safety” was the lowest factor [3,15]; however, in this study, “coping with psychiatric problems” was followed by “environmental safety” and “infection-fall-ulcer prevention”. This difference indicated that more preventive PSMA was performed to manage the hospital environment and prevent infection during the COVID-19 pandemic. Another reason is that patient safety management is a vital evaluation item in psychiatric institutions’ accreditation evaluation standards [16]; thus, patient management activities are steadily being performed. Certification evaluations of actual medical institutions have been shown to have a positive effect on nurses' patient safety awareness and activities [15,21].
Patient safety culture awareness had the highest impact on PSMA (35.3 %), and among the sub-domains, communication and procedures, incident reporting frequency, and hospital environment were significant factors. In Kim and Lee’s [3] study on psychiatric nurses, communication and procedures, patient safety, frequency of incident reports, and direct supervisor/manager attitude were significant influencing factors with an explanatory power of 35 %, showing similar results. Communication and procedures are key factors in PSMA, and they are important factors that affect nurses’ reporting of all patient safety incidents [2,22]. The frequency of accident reports was the second highest in both this study and that of Kim and Lee [3], which means that when accidents occur in wards, reports are being made smoothly. It is considered that to report accidents well, an organizational culture, such as a non-punitive organizational culture, anonymity, and open communication, are necessary at the institutional level [23,24]. Hospital environment had the lowest average among the sub-domains of PSCP, but was a factor influencing nurses’ PSMA. Awareness of the hospital environment was low in most previous studies [1,3,15]. The current study finds that hospital management’s attitude toward patient safety is also a factor that affects nurses’ PSMA, and that hospital management’s active interest and intervention in patient safety are required.
Finally, in this study, “sense of safety control” averaged 3.75 out of 5 points, and was an influencing factor in PSMA. This supports prior results; however, the score was higher in this study than in previous studies (3.40~3.58) that targeted operating room nurses and general hospital nurses using the same tool [11,25]. However, no studies have previously been conducted on safety control among psychiatric nurses, thereby making comparisons difficult. Safety control was higher in the group that had received patient safety education and experienced more accidents [10]. Therefore, to increase safety control, it is necessary to continuously provide patient safety education and experience in psychiatric wards.
Based on these results, we make the following suggestions. First, we found that there were more PSMAs when there was no or a few accident reports during the past year. This was inferred from the results of the preventive activities and medical institution certification evaluations in the corona situation. This is suggested as a follow-up study for more accurate cause identification. Second, safety control variables were used for the first time for psychiatric nurses. Further research related to safety controls is suggested. Third, to prevent patient accidents in psychiatric wards, it is suggested to create a culture in which in the event of an accident, free and active communication between medical teams and non-punitive feedback are given and received. Fourth, this study targeted psychiatric nurses working in 9 psychiatric hospitals across 3 regions. However, there are limitations, in that the hospital’s size and accreditation are not considered. Future research considering the characteristics of hospitals is recommended.
CONCLUSION
This study revealed that organizational PSCP and a personal sense of safety control were factors influencing PSMAs among psychiatric nurses. Among these, PSCP had the greatest influence on PSMA. To improve this, it is necessary to strengthen communication among employees, actively report accidents. In addition, hospital managers ought to provide care and intervene in matters that involve patient safety.
Notes
The authors declared no conflicts of interest.
AUTHOR CONTRIBUTIONS
Conceptualization or/and Methodology: Park D-G & An H-J
Data curation or/and Analysis: Park D-G & An H-J
Funding acquisition: No funding.
Investigation: Park D-G & An H-J
Project administration or/and Supervision: An H-J
Resources or/and Software: Park D-G
Validation: An H-J
Visualization: Park D-G & An H-J
Writing: original draft or/and review & editing: Park D-G & An H-J